© 2006 All Rights Reserved. Do not distribute or repurpose this work without written permission from the copyright holder(s).
Printed from https://www.damninteresting.com/cancer-assassins/
In the USA and other developed countries, cancer is presently responsible for about 25% of all deaths. The human immune system employs a network of microscopic sentries to watch for all manner of diseases, including the malformed, rapidly-dividing cells which make up cancer. But sometimes the immune system’s somewhat lackadaisical response to cancer cells allows the rogue cells to overwhelm the immune system, posing a deadly threat to the body.
Conventional cancer treatments such as chemotherapy and radiation therapy can injure and kill these tumor cells, but with an inevitable degree of collateral damage. By way of example, chemotherapy has a therapeutic index of six to one, meaning that one healthy cell is killed for every six cancer cells which are destroyed. Given that tumors can be made up of millions of cells, the incidental damage caused by chemotherapy is considerable. Radiation therapy has the same drawback.
Clearly these radiation and specialized-poison therapies are highly indiscriminate treatments, but they are the best that modern medicine’s cancer-fighting toolbox has to offer. But science is working hard to develop an army of microscopic agents which can hunt down and destroy cancer cells with decisive prejudice: antitumor viruses.
Pitting viruses against cancer cells is not a new idea. In the early 1900s doctors began to take note of the fact that patients’ tumors tended to regress when a patient contracted a viral disease. But there was no means to harness this knowledge, since introducing harmful viruses into an already compromised individual was a dangerous prospect. Much later, in 1956, researchers deliberately introduced adenovirus— the virus responsible for the common cold— into thirty patients with cervical cancer. Many of the tumors shrunk as a result, but once the immune system began eliminating the virus from the patients’ systems the tumors began to grow again.
Normally, when a virus encounters a cell which it can infect, it injects its genetic material into the cell. The cell’s enzymes react to the new genetic material by setting to work replicating it, essentially building copies of the original virus. In most cases, the thousands of resulting viruses then breach the cell membrane to escape, which kills the cell. Each of these viruses can then move on to repeat the process in other cells. Once the invaders are discovered and identified, the immune system usually reacts by raising the body temperature to slow down cell processes (fever), then sending in white blood cells to eliminate the viruses.
Advances in virus-handling techniques are allowing scientists to refashion viruses from agents of destruction into useful instruments. Gene therapy uses specially prepared viruses to deliver genetic payloads into cells; these viruses are preloaded with the desired genes, and they are modified in such a way that they are prevented from multiplying. The viruses then insert the genes into target cells and die off without killing the host cell. But multiple treatments are problematic, since the immune system recognizes the viruses from the previous treatment, and quickly eliminates them. Researchers are now experimenting with immunosuppressant drugs to delay the immune system’s reaction, as well as some physical modifications to the viruses which help them to evade the immune response.

In 1999, scientists used a modified adenovirus to deliver a gene called “p53” to the lung tumors of twenty-five individuals. A malignant cancer cell is often prevented from entering the natural cell-death phase due to a malformed p53 gene, allowing them to outproduce and outlive normal cells. Using viruses to replace the mutated gene with a normal gene reduced or stopped the tumor growth in eighteen of the twenty-five patients. A similar method has been tested in lab animals where viruses indiscriminately deliver a gene which does no harm to normal cells, but causes cancer cells to die. Where chemotherapy offers a therapeutic index of six to one, these methods have demonstrated indexes of about 10,000 to one in the laboratory.
A more recent approach takes advantage of a virus’s main strength: its propensity for replication. Laboratory-built, submicroscopic assassins have been derived from viruses which are modified so they can only infect cancer cells. These viruses can simply be let loose upon the patient, killing only tumor cells until there are none left to infect. Additionally, the viruses can be equipped with genetic payloads which boost the body’s immune response to the cancer; this effect may actually act as a vaccine against future cancer cells of the same type, since the body’s immune reaction to those cells will be increased.
Because every virus can only infect certain cell types, a whole array of customized cancer-killers would be necessary to address a wide variety of cancers. The adenovirus which causes the common cold can be used against many types of tumors, and has shown impressive results. In August of 2000, a team headed by Fadlo R. Khuri of the Texas Medical Center in Houston reported that twenty-five of thirty patients with advanced head and neck cancer responded favorably to a combination of chemotherapy and a modified adenovirus… in fact the tumors in eight patients disappeared entirely. Adenovirus would be useless against brain tumors due to the blood-brain barrier, however a modified herpesvirus— a disease which infects the nervous system— has been tested against brain tumors in human trials with encouraging early results.
Although the modified viruses would have their harmful payloads removed, thus preventing them from causing the diseases which they typically trigger, there are naturally some risks involved in utilizing viruses… particularly those which are tailored to sidestep our immune systems. Such a virus might mutate into something harmful, posing a greater risk than that from which it originated. But with proper research and testing, perhaps those risks can be mitigated to levels similar to that of vaccinations. In time, after years of experiments, testing, and trials, a typical cancer treatment may involve an injection of modified viruses in concert with chemotherapy and/or radiation therapy, with a cure rate near 100%.
© 2006 All Rights Reserved. Do not distribute or repurpose this work without written permission from the copyright holder(s).
Printed from https://www.damninteresting.com/cancer-assassins/
Since you enjoyed our work enough to print it out, and read it clear to the end, would you consider donating a few dollars at https://www.damninteresting.com/donate ?
It appears that coincidentally, researchers at Hebrew University in Israel have made a very recent breakthrough in this area of study.
The Russians have been experimenting with something very similar; a viral bacteriophage. Essentially a virus which finds specific antibiotic resistant bacteria excellent hosts. Infecting and killing them preferentially to other cell types. Obviously this is not to treat cancer but things like MRSA etc. Though the method is startling similar to that in the article. It really is fascinating stuff.
There are problems with using viruses that may mean that they will never be a widespread treatment.
Alan noted the dangers, but there’s also the difficulty of scaling this sort of treatment up for widespread use.
I’m hoping that the engineered nanoparticles like ORMOSIL’s can successfully target cancer like these viruses without the downside.
Stephen Gordon said: “I’m hoping that the engineered nanoparticles like ORMOSIL’s can successfully target cancer like these viruses without the downside.”
Wow, good link Stephen. I hadn’t heard about that alternative.
This article needs more comments. I’m not really sure what to do about that.
Shandooga said: “This article needs more comments. I’m not really sure what to do about that.”
Send out some links to it in e-mails to your pals, thats what I do. ;) DI article Alan, I’ve lost the link, but just read something similar not long ago about a cure for Lupus Erethamatosis; using ones own imuno cells to slow down the inflamation and hystamines. I will try to find some more inf. and then submit an article about Lupus to DI! for your approval. BTW , Love this site!!
That is just awesome that we can figure out how to do that. That’s all I’ve got to say.
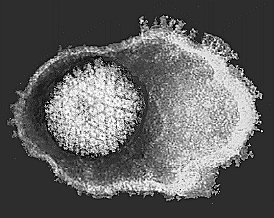
there is something about that second picture that just looks like it tells the whole story. I never thought cells could show emotion, but that second picture looks like those little buggers are just, just…….
beating the ever -loving -shit outta that cell.
Incredible.
If i told you that i had the ultimate cure for all ailments, what would you do/ say?
I want my genetic enhancements, but virus threapy is too dangerous
ORMOSIL’s progress in this area gives me hope.
on the bright side, it didnt say anything about this type of therapy making you lose your hair
…having just lost my mother a little over 4 weeks ago (luckily not to cancer or stroke), I would have to say that anything that can be done to extend the life of a loved one that doesn’t create any additional pain or suffering is worth the risk. We don’t know what we have until it’s gone.
To all of you…during this holiday season, make the most of the time you have here on this green earth and the time you can spend with your parents, family, friends…no matter what type of squabbles you might have with a brother, sister, cousin, etc. “Gone” is forever and irreversible.
Eeps. All I can think of is “Africanized South American Honey Bees”.
Imagine if one of those “dances right past the human immune system” little “cures” happens to have an unexpected/unplanned quirk and ends up not behaving. Bring on HIV2/AIDS2. Let’s all hope they keep those test tubes under an air tight seal.
Not that this comment is relevant to cancer, but last week on the TV show “House”, Dr. Foreman was the patient and contracted an illness from another patients home. They bought more time by subjecting him to Legionaries disease which attacked the original “bug”. Of course they finally figured out what was “bug”ing him but not before the first patient died.
Thank goodness for the doctors who brained up the idea(s) that one virus, deadly or not, could buy more time or even kill off the cancer itself. Damn Interesting stuff.
This reminds me of a recent Dr. Who episode where The Doctor visited a hospital where they discovered the cure to every known disease in the universe by infecting other people with…every known disease in the universe. Yeah I’ll just leave a link to the Wikipedia entry about it.
http://en.wikipedia.org/wiki/New_Earth
Dr. Evil said: “If i told you that i had the ultimate cure for all ailments, what would you do/ say?”
And the guy telling me that has a moniker like “Dr. Evil”? I’d say, “Riiiiiiight!”
another viewpoint said: “…having just lost my mother a little over 4 weeks ago (luckily not to cancer or stroke), I would have to say that anything that can be done to extend the life of a loved one that doesn’t create any additional pain or suffering is worth the risk. We don’t know what we have until it’s gone.
To all of you…during this holiday season, make the most of the time you have here on this green earth and the time you can spend with your parents, family, friends…no matter what type of squabbles you might have with a brother, sister, cousin, etc. “Gone” is forever and irreversible.”
Amen to that. Live like you’ll die tomorrow, plan like you’ll live forever.
Work like you don’t need the money.
Love like you’ve never been hurt.
Dance like nobody’s watching.
another viewpoint said: “…having just lost my mother a little over 4 weeks ago…”
Condolences to you darlin’. Am sure that we all here wish you Peace of mind and Joy this holiday season,& I’m sure your Mom would too.OOO
Still can not find that elusive article on the personal imuno-therapy in re Lupus…will keep researching…Thank you Alan for re-running this DI piece.
Oh & HBDTM tommorow. I am now officialy old enough to fart dust, lol. (sigh)
FIRST!!! (if you minus all previous comments)
Sharks with lasers on there heads are good for removing cancerous growths…the side affect is they can destroy other living cells.
In addition to the unintentional consequences…there are “pseudo-military” applications.
The book, The White Plague, came to mind as I read this article.
http://en.wikipedia.org/wiki/The_White_Plague
I wonder if anyone is actually working on tailored bio-warfare? An abominable thing, but that never stopped anybody.
Alan – you might want to have expanded a little on the term “therapeutic index”, as some of us without a medical degree didn’t get the full import of the term ;>) http://en.wikipedia.org/wiki/Therapeutic_index
I think that the very small chance (less than 1%) that something like this could develop horrible consequences _and_ escape containment is an excellent argument for lunar colonization, terraforming Venus and Mars, and for supporting further development of a Daedalus project. In addition to the naturally evolved horrors like Marburg, Ebola, HIV and WWE, we have a chance (small but existant) that we could create something as bad, plus the danger of an impactor from space. It would be a shame if the human race disappeared (except for lab specimens collected by UFOs) because of economic concerns regarding space travel.
It reminds me of a background story element in one of my favorite books, Walter Jon Williams’ “Aristoi”, where the first Earth was destroyed by runaway nanotechnology that used all matter on Earth as building material, then fed upon itself until nothing was left but inert foam.
The missing paragraph of my above message (due to the less than symbol being a problem here) was as follows:
I think that the very small chance (less than 1%) that something like this could develop horrible consequences _and_ escape containment is an excellent argument for lunar colonization, terraforming Venus and Mars, and for supporting further development of a Daedalus project. In addition to the naturally evolved horrors like Marburg, Ebola, HIV and WWE, we have a chance (small but existant) that we could create something as bad, plus the danger of an impactor from space. It would be a shame if the human race disappeared (except for lab specimens collected by UFOs) because of economic concerns regarding space travel.
Hey Drakvil… sorry about the bug. I fixed your original comment to re-insert the missing paragraph so it makes sense.
Tink said: “I am now officialy old enough to fart dust, lol. (sigh)”
Is that similar to pixie dust?
I didn’t know that there was a minimum age for residents of neverland to do that…
LOL, yeah baby, thats right. No sparkles. Thanks for the laugh, I sure needed that!
If people are interested, the reason most chemotheraputic agents have such a low theraputic index is due to the fact that they are not targeted agents. For example, the one of the most common classes of chemotherapy drugs is that of DNA-alkylating agents. These compounds, the best-known of which is Cisplatin or cis-diamminedichloroplatinum (II), work by damaging DNA in all cells that take up the compound. Cisplatin forms an adduct (bump) on DNA wherever there are two consecutive guanine nucleotides; whenever a cell tries to replicate or transcribe this DNA, the polymerase is stalled and eventually the cell, cancerous or not, kills itself. A drug like paclitaxel (taxol) works by preventing microtubule growth in all cells that take it up, preventing chromosomal positioning in mitosis, again leading to cell suicide (apoptosis).
These chemo drugs work as anti-cancer therapies almost solely because cancer cells replicate faster, triggering the errors in replication that lead to the cell death at a higher rate than normal cells, which are often more proficient in cell or DNA repair, with active checkpoint controls. Given the indiscriminant nature of many of the strongest cancer drugs, it is akin to a race to see whether a chemo treatment can destroy a tumor before the treatment causes irreparable damage to an important organ, necessitating a change in treatment.
Many of the newer treatments attempt to target tumors specifically. Anti-angiogenesis therapies, such as the Avastin (an antibody against a common vascular growth factor) fall into this catagory.
Inserting a gene into a “mollified” adenovirus is the most common approach to gene therapy, which I have always found curious given its lack of a lysogenic cycle. p53 (THE antitumor protein) is a good gene to insert, although one could make an argument for inserting MDM2.
However, and this is extremely important to note, viruses are VERY poor at preventing DNA errors during replication. Adenoviruses are dsDNA viruses, and are thus not nearly as prone to errors as retroviruses are, so the likelihood of a cancer-fighting virus forming the next HIV is negligible. However, the fact that this virus inserts cancer-related DNA makes for a serious concern that it could mutate to actually insert oncogenes or proto-oncogenes. A mutated p53 gene could realistically code for a mutated p53 protein that suppresses expression of “working ” p53 proteins while not actually fighting cancer. This would actually increase the likelihood of someone developing cancer. While its benefits might be immense, gene therapy is serious, dangerous stuff.
Oh, and my favorite term: Okazaki fragments.
I think that the fact that we are headed into a new way of thinking and using new medical technology to curing cancer is going to be great.
My family has a rampant history of cancer, and many of the family members that I have lost to cancer were dear to me. Most recently my Grandfather died of lung cancer in late december.If this treatment were available, and could have saved him and any other of my relatives, that would have been awesome.
Other creative alternatives to viruses:
Injection / Injestion of chemicals only absorbed into cancer (or normal) cells, followed by Injection / Ingestion of chemical / virus that kills cancer when combined with or not combined with other chemical to protect normal cell or destroy cancer cell.
An umbrella cure would be difficult since there is a different type of cancer for just about every cell type that exists, but I wouldn’t rule out the possibility of such a cure or treatment anyway.
Combination treatments, w/ chemo / radiation.
What if you gave the cancer cancer? That might not work, since cancer affects the larger organism and not necessarily neighboring cells cells. But what if you could predictably mutate the cancer into something less aggressive. Nevermind…
How about water poisoning – overhydration? Might waterlogging less robust cancerous cells slow down their reproduction.
Or maybe dehydrating… or over-salting. Don’t know what the theraputic index would be for that.
Targeted body temperature manipulation? Would that do anything? Cooling or heating of cancerous/noncancerous regions for extended periods of time?
Or a new application for E.C.T. (electroconvulsive therapy), more focused on finding a low current, targeted frequency than shocking the crap out of everything. Could you find the resonant frequency of a cancerous cell, simultaniously using a salt to aid in the process?
Ultrasound therapy? Do they have that yet?
High pressure? Low pressure? Pressure flux?
To get sort of sci-fi, how about using antimatter? I know a guy who experiments with it, but producing it is a bitch.
I have no idea; just wondering what has already been attempted.
Did anyone see that new movie with Will Smith in it … yeah there are risks
Hello Mr. Bellows
Please exuse my previous double post learning curve met :)
Dear Mr. Bellows I have been a huge fan of damn interesting since i first hear of your sight ether through npr News radio or through some obsucre new story i read on the net or heard on the tv. I think i have read of of the storys you and your writers have written. The dangers of oxygen, the cancer fighting drugs of our own imune systems creating and every other Damn intersting thing you and your writers have to put on digital canvas or as you say ” Dead tree flesh” Alien hand syndrome for the win. Many of these storys , and treasures have lead me to hours of reading and sometimes book purchases. I would like to thank you and your writters your staff and all the people help you do this work of beaming bright lights of wisdom and explanation, history science, and every other bit of damninteresting information into my head and the heads of the friends i constantly tell about your Site. Damninteresting for ever. Thankyou
Cancer murdered my mother.