© 2018 All Rights Reserved. Do not distribute or repurpose this work without written permission from the copyright holder(s).
Printed from https://www.damninteresting.com/the-curse-of-konzo/
On 21 August 1981, Australian physician Julie Cliff received the following message on her telex, a print-on-paper precursor to modern text messaging:
“Polio outbreak. Memba District. 38 cases. Reflexes increased.”
The apparently routine message was sent from the Provincial Health Directorate in Nampula, a city in northern Mozambique. Cliff worked in the epidemiology department of the Mozambican Ministry of Health in Maputo, at the southern end of the country. Effective vaccines against poliomyelitis—a food and water-borne infectious disease that can damage nerves and cause paralysis—had been developed in the 1950s and 1960s, eliminating polio from many industrialized countries. However, the disease remained rife throughout sub-Saharan Africa. So the message was unremarkable—except for one thing. In the acute phase of polio, tendon reflexes are not increased. They are absent.
Only a few possible reasons could account for this inconsistency: flawed examination of the patients, a typo in the telex, or some unknown disease process causing an unusual pattern of paralysis in the unfortunate Mozambicans.
Dr. Cliff arrived in Nampula province shortly afterwards as part of a small Health Ministry investigation team, determined to get to the root of the mystery. Typographical errors and poor clinical examination technique were quickly ruled out as possible explanations for the anomaly. Close inspection of affected individuals confirmed the disease was definitely not polio. Yet the question remained: what else could it be?

Other doctors already at the scene included a young medic from Sweden named Hans Rosling, who was working in one of the affected areas as a District Medical Officer. When first confronted with a line of women and children suffering various degrees of paralysis, he reached for the biggest neurology textbook he could find. “Their disease did not exist in that book,” he later recounted. Lacking other ideas, Rosling was soon forced to entertain a disturbing possibility: biological or chemical warfare.
The notion was not so outlandish. At the time, the new nation of Mozambique was in the early stages of a bitter civil war. Forces loyal to the socialist ruling party Frelimo (Frente de Libertação de Moçambique)—supported by the Soviet Union—were battling the anti-Communist Renamo organisation (Resistência Nacional Moçambicana), sponsored by the apartheid-era South African and Rhodesian governments. In this edgy and complex, post-colonial, proxy-Cold War situation, rumours proliferated and almost anything seemed possible. Residents reported sightings of a South African submarine off the Nampulan coast a few weeks prior. Rosling’s suspicions of skulduggery were sufficiently strong that he packed his young family into a car and sent them to the safety of the nearest city, while he stayed to continue his work.
In the days that followed, no evidence for any kind of biological or chemical attack emerged. Nevertheless, cases of the mysterious paralysis continued to mount. Each followed a troubling pattern: the disease usually affected women and children, almost invariably in rural villages that had already endured months of a severe drought. Typically, it would strike quickly, over a matter of days or even hours. Previously active young mothers and children would go to sleep with little inkling of anything amiss, only to wake the next morning with various degrees of muscle stiffness and contractions in the legs, and—less commonly—in the arms, too. Sometimes a bout of heavy exertion, such as collecting water for the household from a distant well, seemed to trigger symptoms the next day. Affected people would find themselves unable to walk normally or, in the worst cases, at all. It was almost as if someone—or something—had tied their legs together with invisible cord.
The affliction appeared to be irreversible. As the number of paralysed people grew, the investigators worked with increasing urgency, travelling to remote parts of the province to examine potential cases, interview members of local communities to establish possible causes for the disease, and take blood samples for laboratory analysis.

Initial indications favoured a microbial origin for the condition: if not polio, then some other pathogen. Many early case reports described symptoms such as fever, headache, and diarrhoea preceding the onset of paralysis—symptoms consistent with an infectious disease. Likewise, the clear clustering of cases in small communities and family groups pointed to person-to-person transmission. After all, Africa hosted many unpleasant and little known parasites, bacteria, and viruses—such as the newly emerged Ebola virus, first identified in Sudan and Zaire in 1976.
But subsequent investigations revealed no obvious pathogens. After several days in the field Cliff’s team withdrew to Maputo to regroup and consult with international experts, including those from the World Health Organization. Telex machines from Mozambique to Geneva chattered with criss-crossing hypotheses, while blood samples were hastily despatched to specialist labs overseas, including the British biological and chemical weapons research centre in Porton Down, England.
The team perused a series of increasingly dusty and dense printed journals and textbooks. They identified two diseases with possible relevance to the Nampulan outbreak. One disease, called lathyrism, produced a very similar clinical picture: upper motor neuron damage leading to increased muscle tone and paralysis. Lathyrism typically occurred on a sporadic basis in south Asia, but was also noted among the detainees of Vapniarka, a concentration camp in Romania, during World War II. The other disease was an obscure neurological disorder named Tropical Ataxic Neuropathy, or TAN, first reported in Jamaica in 1897 but since described in a number of other countries scattered across the tropics, including another East African country, Tanzania.
Intriguingly, both diseases were nutritional, rather than infectious, in nature. With lathyrism, the illness was caused by a toxin present in certain legumes—including the livestock peas that were the sole foodstuff allowed to the unfortunate Jewish internees in Vapniarka. However, none of these legume species were grown or consumed in northern Mozambique. The purported cause of TAN was more vague—even a century after its discovery, the exact cause is unknown, although nutritional deficiencies have been proposed as possible factors, and experts had long linked it to a food crop widely cultivated in Mozambique and elsewhere. But the symptoms of TAN—which include blindness, hearing loss, and an unsteady gait—bore little resemblance to the distinctive paralysis the doctors saw in Nampula province.

Meanwhile, infectious disease experts in Maputo remained convinced that an unidentified virus was the culprit. They suggested further investigation of insect disease vectors in the affected areas. The team dutifully added questions about insects to their interview questionnaires, and went back into the field. It emerged that lots of mosquitoes and bedbugs bit people in affected communities—but lots of mosquitoes and bedbugs bit people in unaffected communities, too.
By the end of September 1981, Cliff’s team—now expanded to include Dutch botanist Paul Jansen—was no longer looking for a contagious disease. They had considered and excluded all known infectious agents that could possibly perpetrate the perplexing plethora of paralysis. Nor had detailed analysis of various bodily fluids demonstrated any unknown ones.
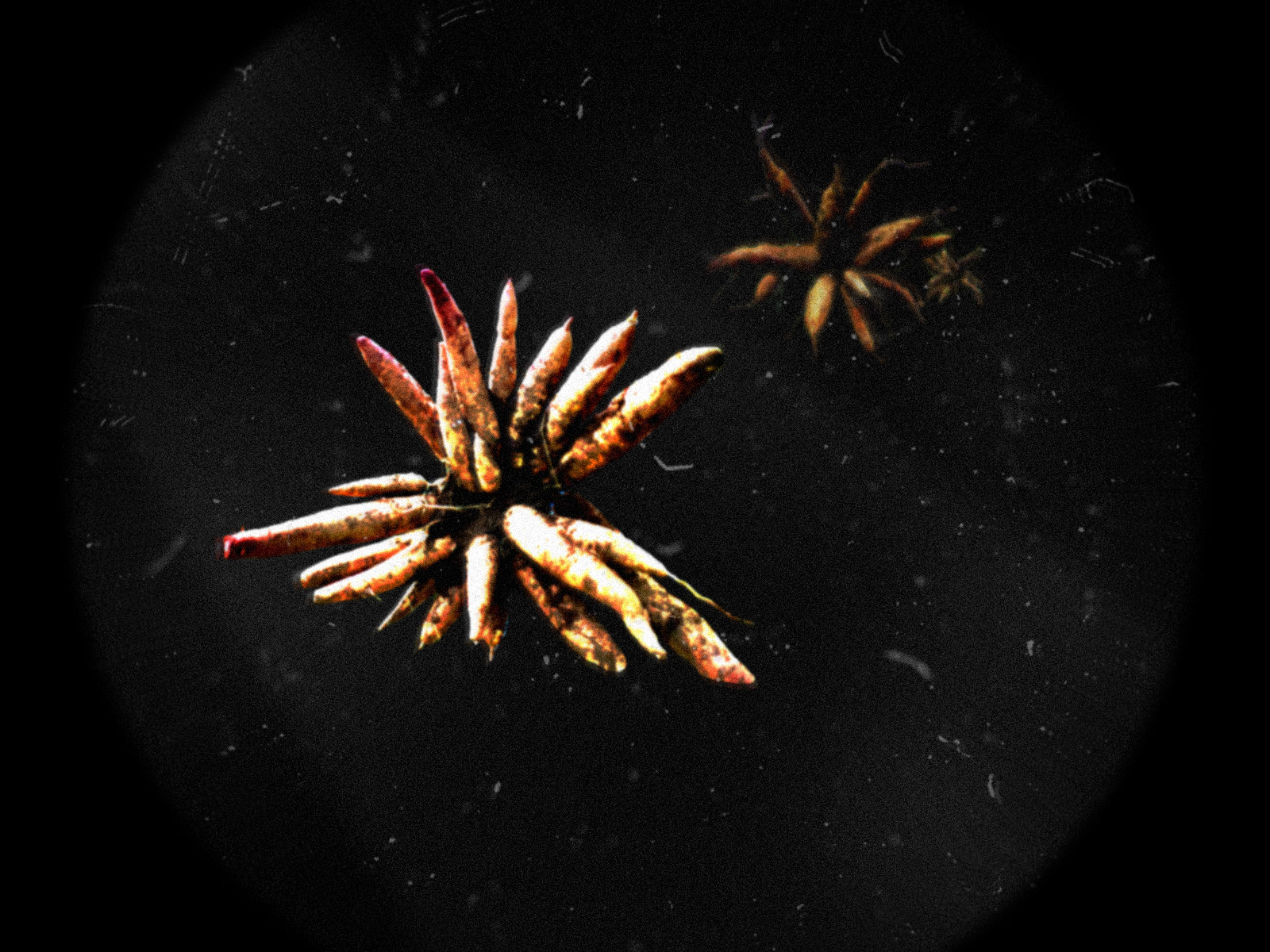
The investigators’ attention turned back towards dietary factors. Despite the drought, the problem wasn’t a lack of food. While many local people had suffered, few actually starved and unlike later famines elsewhere in East Africa, mortality was low. Much of the credit for this could be attributed to a single plant species that had come to the rescue: Manihot esculenta, also known as ‘cassava’.
Cassava is a small tropical shrub that produces a starchy and edible underground root. It was originally cultivated in Latin America and the Caribbean, but was introduced to Africa in the 16th century by the Portuguese. It subsequently spread throughout the tropics and beyond. The versatile tuber can be processed into a starchy powder exported to temperate regions, where it is known as tapioca, and used to make pudding. In many ways, cassava is an exemplary food, whose virtues are particularly relevant to Africa. Notably drought- and pest-resistant, cassava thrives in marginal soils incapable of supporting other crops. Although it lacks protein, it is a good source of calcium and vitamin C, and an exceptional provider of energy. Indeed, of all the main staple food crops, cassava yields the highest number of calories per area cultivated, making it invaluable on a continent still stalked by famine.
In rural Mozambique, as in much of Africa, people often grow cassava on a small-scale basis close to households as a “crop of last resort,” for consumption when they lack other food sources in the hungry season—or in times of conflict, crisis, or drought. Cassava comes in “bitter” and “sweet” (or, more accurately, “not bitter”) varieties, with the bitter types particularly valued for their resistance to locusts and other herbivores.

Early in the investigation, an elderly man in one of the affected villages told the doctors, “This disease has happened because the rain has not washed our cassava.” Perhaps understandably, investigators initially ignored him. The practice of disease outbreak investigation involves an established sequence of steps concerned with relating cases to “time, place, and person.” Heeding advice from grizzled old locals does not feature prominently in field epidemiology manuals.
However, as each new test failed to yield evidence for any old or new pathogens, the investigators returned to the old man’s words. Cassava was an important element of the local diet in Nampula, and therefore hard for Cliff and her team to overlook if they were considering a nutritional cause for the puzzling paralysis. The doctors formulated a worrying hypothesis involving one of humanity’s most feared poisons—a substance that disrupts the body’s utilisation of oxygen at a cellular level, and formed the principal ingredient of the notorious Zyklon B gas used in the Nazi extermination camps: hydrogen cyanide.
One clue was the fact that cassava often leaves a bitter taste in the mouth. This bitterness derives from two types of sugar molecules: linamarin and lotaustralin. These molecules are termed “cyanogenic glucosides,” meaning that in certain circumstances—for example, when exposed to the enzymes and bacteria of the human intestine—they will decompose and produce hydrogen cyanide. The more bitter the cassava, the greater the potential exposure to cyanide.
Sure enough, when Jansen tested a range of foodstuffs from the disease-affected areas, he found high levels of cyanogens in the cassava samples. And when the team tested blood samples from affected people for thiocyanate—cyanide’s breakdown product within the human body—the average result was 20 times normal levels. The researchers now had to entertain the possibility that the food that saved so many Mozambicans from starvation was, in some cases, paralysing them.
With a plausible hypothesis to test, the application of tried-and-tested disease outbreak investigation methods started to yield results. When Cliff and her colleagues related the pattern of cases to time, they realised the August peak of the epidemic corresponded closely to the region’s main cassava harvest. When they mapped out cases by place, they saw that the disease largely spared coastal areas, which was consistent with their understanding of the local diet: access to fish and to food markets meant people depended less on cassava. Finally, when the team looked closely at “person,” the preponderance of the disease in women of childbearing age and children over the age of two also made sense: in rural Mozambique, as in much of Africa, women prepare food for the household and they, with their accompanying children, would be most exposed to cassava during processing and consumption. Men are usually privileged with more diverse dietary pickings, and are spared the additional nutritional stress of pregnancy and breastfeeding. Furthermore, the extreme food shortage caused by the recent drought had forced many women to eat something that would normally be thrown away: cassava root peel, which Jansen’s tests had shown to harbour particularly high levels of cyanogens.

With the warm glow of hindsight, it may seem surprising that the investigators did not realise the connections earlier: a number of commonplace foods are known to contain cyanide, cassava among them. Outside of the tropics, one of the better known examples are bitter almonds. In crime fiction, their aroma traditionally emanates from fresh corpses as a sign of villainy afoot. For most of us, the distinct odour of bitter almonds is indeed the scent of cyanide, but up to 40 percent of the population—presumably including a few unfortunate detectives—have a complete genetic inability to smell the poison. Many wild varieties of the almond tree express the bitterness trait—determined by a single recessive gene—and produce these deadly seeds; it has been estimated that consumption of around a dozen will kill an average person. The seeds of many other familiar agricultural plants also contain cyanogens, including apricots, cherries, peaches, plums, and even apples. The growing tips of sorghum, a traditional crop domesticated in Africa long before the arrival of cassava, contain high levels of cyanogens, while some of the very highest levels—up to 8,000 mg of hydrogen cyanide per kilogram—are found in bamboo shoots.
Nonetheless, very few people who eat these foods suffer adversely from cyanide exposure. In many cases, cyanogen levels are extremely low in the specific varieties consumed—the whole almonds found in grocery stores almost invariably belong to the sweet type, rather than the bitter, for example. And the part of the plant makes a difference: while the stones and pips (“pits” and “seeds” for North Americans) of various fruits may cause illness if chewed and swallowed in large quantities, such seeds are usually discarded before consumption, or excreted intact and undigested. With sorghum, it is the cyanogen-less grain that people eat, rather than the young leaves—although the latter have been known to poison grazing livestock. With bamboo shoots, research revealed substantial variation in the levels of cyanogens found in the various species of edible bamboo, but standard processing and cooking methods effectively eliminate the toxin in almost all cases. As always, there are exceptions—an account of an unusually fatal bamboo pickling incident in Thailand was published in 2011—but safety can normally be assured by means of a thorough stir fry.
Much of this background was familiar to Cliff and her team in 1981—so they knew that in theory, at least, the cyanide in cassava should not have posed a significant threat to human health. Furthermore, there were at least a couple of conditions already attributed to cyanide ingestion, but neither were anything like the illness the doctors saw in Nampula province. First, there was the well-established progression of symptoms seen in acute cyanide poisoning, which include vomiting, diarrhoea, seizures, coma, and ultimately, death—but not normally paralysis. Second, there was Tropical Ataxic Neuropathy, the disease that the team had read about in Maputo. TAN had long been linked to cassava cultivation, and at the time was also hypothesised to be linked to cyanide exposure. But in both cases, the entirely different pattern of symptoms threw the investigators off the bitter scent.
Doctors even lacked an established name for the “new” disease. Initially, they used the local Mozambican word—mantakassa—but it was later discovered that an Italian physician, Giovanni Trolli, had identified the same pattern of symptoms in the 1930s in rural areas of Kwango province in the then-Belgian Congo. While Trolli did not establish the cause of the symptoms at the time, he collated reports from several other doctors in the region over a two-year period and recorded the local Congolese name for the condition: khoondzo, or “konzo.” The word meant “tied legs” and was also the name given to a talisman and a trap used by people in the area to ensnare wild animals. Although separated by nearly 50 years and more than 1,000 miles, the two diseases were clearly the same. Eventually, the all-too-appropriate name “konzo” prevailed.

When the researchers looked beyond Africa, another mystery became apparent: konzo’s geographical distribution does not map neatly onto areas of cassava consumption. Half a billion people living across the tropics rely on cassava as an important part of their diet, yet in global terms konzo is, thankfully, a rare disease. It has never been reported in the Americas, where cassava was first domesticated, nor in Asia, where it has become an important staple crop in many areas. Cassava is widely consumed in West Africa—and grown on a commercial scale in countries such as Nigeria—but konzo has never been documented in this region.
For cassava, as with almonds and bamboo shoots, it seems that much depends on the particular variety of plant grown and the circumstances surrounding its preparation. In Asia, people tend to only cultivate the “sweet” cassava varieties, so starting concentrations of cyanogens are low. In the Americas, traditional processing methods—such as the “tipiti” plaited sleeve press used by Amazonian tribes—are highly effective at removing cyanide, although they require large volumes of water. In Africa, different areas rely on different processing techniques. In central and eastern Africa, the preferred method involves soaking peeled cassava roots in water for three days, followed by a period of sun drying, before pounding the resulting product into granules or flour. But when drought and hunger intervene, soaking and drying times are cut short.
Even then, the resulting cyanide exposure should not be sufficient to cause konzo in normal nutritional circumstances. Adequate intake of sulfur amino acid-containing protein helps the body metabolise and excrete cyanide, but cassava’s low protein content—and often, a lack of access to meat, fish, and other protein-rich foods—means that cassava-dependent communities may not be able to maintain this basic dietary defence. Compounding this problem, in times of drought, bitter cassava becomes even more bitter: the water-stressed plants concentrate additional cyanogens in their leaves and roots to deter insects and other animals who might otherwise be sorely tempted by such a convenient “crop of last resort.”
By the end of the October 1981, Cliff and her colleagues had collected and connected the most important pieces of the Nampulan paralysis puzzle. They were certain that the disease was associated with the high levels of cyanide found in affected individuals. The cyanide came from the bitter cassava that was—thanks to an unfortunate collision of socioeconomic, botanical, and meteorological factors—the defining feature of the local diet. However, the exact biochemical and neurological chain of causation remains uncertain to this day. Konzo can be considered a form of chronic cyanide poisoning, but it is still unclear why its symptoms differ so much from those of acute cyanide poisoning—and what relationship, if any, konzo has with those other mysterious nutritional diseases, lathyrism and TAN. Occasionally, people in drought-stricken, cassava-dependent areas indeed display symptoms of acute cyanide toxicity. Reports of these early symptoms may have initially misdirected Cliff and her colleagues toward considering an infectious cause for the disease, but the onset of konzo itself usually occurs much later, after weeks of excess and near-exclusive cassava consumption.

As the regional diet diversified in the months following the 1981 cassava harvest, the incidence of konzo in Nampula province slowed and eventually stopped. The Health Ministry investigation team dispersed. Julie Cliff returned to Maputo. Hans Rosling left his job as a District Medical Officer later that year but maintained a strong interest in konzo, going on to write his Ph.D. thesis on the disease. Jansen returned to botanizing, co-authoring a tome on the traditional use of medicinal plants in Mozambique published in 1983, before expanding his ethnobotanical interests ever further across the tropics: he later became instrumental in projects to catalogue the traditional plant resources of both Southeast Asia and tropical Africa. Meanwhile, the rains returned to northern Mozambique for the 1982-83 growing season, providing water to soak the cassava and yield a safer harvest for the local population.
Over the following decades, Cliff, Rosling, and others identified more konzo clusters in several countries in central and eastern Africa. They ultimately diagnosed more than 1,000 cases in the 1981 Mozambique epidemic—a similar number from Trolli’s original 1936-37 Congolese outbreak. Researchers believe that the cumulative number of cases reported officially in Africa—around 11,000—represents a gross underestimate, largely because of poor access to health care—and hence poor case-reporting—in vulnerable regions. In the now-Democratic Republic of Congo alone, estimates go as high as 100,000 cases. Here, in particular, it remains a significant ongoing problem: decades of conflict have lumbered the population of this repeatedly re-named country with a legacy of social and economic problems, making it vulnerable to nutritional diseases like konzo.
For individual konzo sufferers, treatment options are minimal. The muscles in the legs tighten and contract to a varying extent (“spastic paraparesis,“ or “tetraparesis“ if all four limbs are affected). In mild cases, people can still walk unaided, albeit with the tiptoeing “tied legs” gait that gives the disease its name. In moderate cases, crutches or walking sticks are needed. In severe cases, people’s legs are completely paralysed (“spastic paraplegia“). Physical therapy can help people manage their symptoms, but the motor neuron damage is irreversible. This is particularly devastating in societies with very little formal health or social support—where physiotherapy, for example, is not widely available, and where income is often earned via physical labour.

However, in 2004, it was discovered that the disease is completely and easily preventable. A recently retired Australian plant scientist named Howard Bradbury discovered that an additional step in cassava processing—namely, wetting cassava flour with water and leaving the resulting paste to stand for five hours—would greatly reduce cyanogen levels. As long as the gloop contains sufficient linamarase, a natural enzyme that should be present in the flour anyway, and there is adequate ventilation to allow the safe outgassing of hydrogen cyanide, the procedure—not too dissimilar, of course, from the “rain-washing” the old man in Nampula had described—will nearly always reduce human cyanide exposure to safe levels. Subsequently, Bradbury discovered that in direct sunlight, the enzyme works even faster: just two hours will suffice. The water requirements are modest, and field trials in east and central Africa have shown this “wetting method” to be practical, effective, and widely welcomed by women in vulnerable villages.
The story of cassava and konzo should not alarm global connoisseurs of tapioca pudding, bamboo shoots, and sweet almonds. It demonstrates that well-nourished, well-educated, and wealthy people generally have very little to fear from eating potentially cyanide-containing food plants. Only a sustained period of consumption of large amounts of inadequately prepared bitter cassava—which only occurs in conjunction with a collection of other disagreeable social and environmental circumstances—causes the disease. In short: only poor people suffer the curse of konzo.
© 2018 All Rights Reserved. Do not distribute or repurpose this work without written permission from the copyright holder(s).
Printed from https://www.damninteresting.com/the-curse-of-konzo/
Since you enjoyed our work enough to print it out, and read it clear to the end, would you consider donating a few dollars at https://www.damninteresting.com/donate ?
1st! DI as always!
Very – no, damn interesting! :)
Damn Interesting, well done Matt… very easy to follow along and understand
Great article! Just the right mixture of describing high-level impact and details to keep it interesting and informative.
DI as always. I work in QA and these kind of “I should have known that” answers are often right below the surface. They are handed to you early on by someone who is not considered smart enough to have any input. Then in 2004, some genius plant scientist “discovers” the wetting method. Which is exactly what the “grizzled old local” meant by the poorly translated, “This disease has happened because the rain has not washed our cassava.” Most likely, the tribal knowledge was to beat the cassava to powder, put it out to dry, and not eat it unless it had been rained on at least once.
Mr. Castle:
Superb article – clearly up to the high standards of DI.
Your article also makes me wonder how much of the way I feel is due solely to my diet.
I make a great effort to eat clean, nutritious foods, but, in all actuality, who knows just exactly how safe our food supply is?
Good job Matt!
Love the alliteration:
“possibly perpetrate the perplexing plethora of paralysis”
Nice!
One small typo:
“The doctors formulated a worrying hypothesis”
I think you mean working hypothesis.
“With the warm glow of hindsight,…”. I love that phrase.
Well done, Mr. Castle. Damn interesting indeed!
“Rosling’s suspicions of skulduggery were sufficiently strong that he packed his young family into a car and sent them to the safety of the nearest city, while he stayed to continue his work. ” Typical Swede, pointing the finger at South Africa without a shred of evidence.
I love this site, and I have encouraged others to read it. I bought the book, loved it -of course- and gave it to others to read. However, damnintersesting has become, mostly, a hub for interesting articles written by others; which are great, and I’m very thankful.
Why is this site so resistant to advertising? It seems hypocritical to be redirected to another which demands eventual subscription or where the reader is subjected to the same advertising anyway.
Very little original content is being provided by damninteresting; why not accept advertisements?
Wouldn’t that be in everyone’s best interest?
Checking back in after 13.5 months.
As am I, after being unable to read many articles without payment or subscription.
“possibly perpetrate the perplexing plethora of paralysis”
Rather flippant writing for such a serious topic, don’t you think?
great article
SecureEduardo:
Welcome back.
SecureEduardo:
Good to see you that you’ve returned!